December 5, 2019
Expanding opportunities for participation, CMS outlines the new MIPS Opt-In Policy for the 2019 performance year
For the 2019 Merit Based Incentive Payment System (MIPS) performance year, the Centers for Medicare and Medicaid Services (CMS) chose to expand MIPS eligibility requirements. To be classified as a MIPS eligible clinician, providers are required to satisfy the following three low volume thresholds:
- Bill more than $90,000 for Part B covered professional services
- See more than 200 Part B patients
- Provide 200 or more covered professional services to Part B patients
To expand opportunities for providers to participate in the MIPS program, clinicians who exceed one or two of the low-volume thresholds can now opt in to the program and potentially earn a positive payment adjustment that would begin in 2021. As an example, if a provider sees more than 200 Part B patients and provides more than 200 covered professional services to part B patients but does not bill more than $90,000 for covered professional services to Part B patients, they would not be eligible for MIPS under the standard eligibility criteria but can opt-in to the program. Eligible clinicians and groups that opt in to MIPS will be evaluated under the same criteria as other program participants, which could result in either a positive or negative payment adjustment.
Verifying Opt-In Eligibility
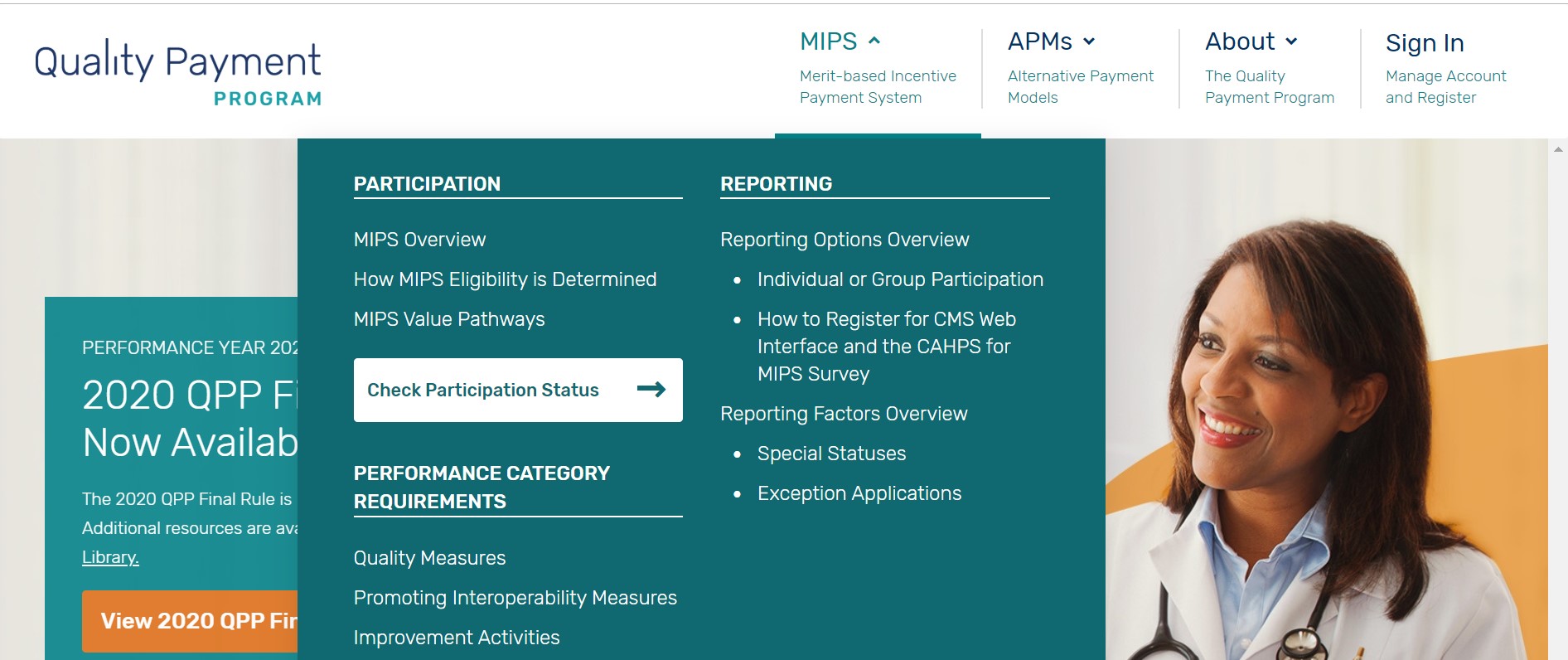
To determine eligibility, clinicians should visit https://qpp.cms.gov/participation-lookup to verify MIPS eligibility for performance year 2019. Under the MIPS tab, providers will see the option to “Check Participation Status”. After entering their provider specific NPI, MIPS eligibility should be listed. Those clinicians eligible to opt in to MIPS will see whether they are eligible to opt in as an individual and/ or as a part of a group reflected under “MIPS eligibility.”
Making an Opt-In Election
The ability to make an opt-in election will be available on qpp.cms.gov upon the opening of the MIPS data submission window in early 2020. To complete an opt-in election, providers must first set up an account for the Quality Payment Program website. Providers will be required to make their opt-in election prior to submitting their MIPS data for the 2019 performance year. Once a provider has elected to opt in the decision is final, and the election may not be revoked.
More Information
- To verify your MIPS eligibility, please follow the link here.
- To access the CMS fact sheet on the MIPS Opt-in Policy please click here.
- To learn more about the 2019 MIPS Requirements, please click here.
- To access the MIPS opt-in toolkit, please click here.
- To learn more about “What is MIPS”, please click here.
