December 20, 2024
Preparing for MIPS: Your 2024 End-of-Year Check-In

The Merit-based Incentive Payment System (MIPS) is one of the available pathways for providers and healthcare practices to participate in the Quality Payment Program (QPP), a federal program designed to reward MIPS-eligible clinicians and practices for improving the quality of their patient care and patient outcomes. Under MIPS, the Centers for Medicare & Medicaid Services (CMS) evaluates your performance across 4 categories during the MIPS performance period (January 1, 2024 to December 31, 2024):
- Quality
- Promoting Interoperability
- Improvement Activities
- Cost
Your performance across these categories is used to calculate a MIPS final score of 0 to 100 points.
Your MIPS final score will determine whether you receive a negative, neutral, or positive MIPS payment adjustment to your Medicare Part B claims, applied during the MIPS payment year (January 1, 2026, to December 31, 2026.)
The 2024 MIPS performance year has brought numerous changes to MIPS Quality measures. Success in the MIPS program requires participants to ensure that their EHRs and MIPS reporting systems have been updated with the most recent MIPS Quality measure information and requirements. Success also requires you to ensure accuracy in your data collection and reporting. In this article, we will walk you through an end-of-year MIPS check-in that will help prepare you as the 2024 MIPS reporting deadline approaches.
Preparing for MIPS: What you need to do
1. Check your current MIPS eligibility
Individual MIPS eligibility is determined by several factors, including clinician type, date enrolled in Medicare, and the volume of care provided to Medicare patients. You are considered a MIPS-eligible clinician—and are required to report—if you are an eligible clinician type; enrolled in Medicare before January 1, 2024; you’re not identified as a Qualifying Alternate Payment Model (APM) Participant (QP); and you exceed the low-volume threshold criteria. Clinicians who do not meet the criteria for eligibility are not eligible to receive MIPS payment adjustments in the associated payment year. However, they may still participate voluntarily in traditional MIPS to receive performance feedback.
You can confirm your current MIPS eligibility, either as an individual or as a group, in one of 2 ways:
- Entering your National Provider Identifier in the QPP Participation Status Tool, or
- Signing into the QPP website to check eligibility status for all groups you’re associated with and the connected clinicians in your practice
An indicator of individual and group eligibility status can be found beneath each practice association. You can view additional information about MIPS participation (e.g., reporting requirements, reporting and participation options, and payment information) and eligibility by clicking “+ Expand.”
2. Understand your reporting requirements
Three reporting options are available to MIPS-eligible clinicians to meet MIPS reporting requirements, each with associated reporting requirements.
Traditional MIPS is the original reporting option. For this option, you select which Quality measures and Improvement Activities to report from all available options. You will report the complete measure set for the Promoting Interoperability performance category. (You are not required to report data related to the Cost category, as CMS collects and calculates Cost-related data.)
MIPS Value Pathways (MVPs) is the newest reporting option, offering clinicians a more meaningful and reduced group of measures and activities relevant to various specialties or medical conditions. For this reporting option, you select the MVP most applicable to your practice and choose from the available Quality measures and Improvement Activities; as for Traditional MIPS, you are required to report the complete Promoting Interoperability measure set and are not required to report data related to the Cost performance category.
The APM Performance Pathway provides a streamlined reporting option for clinicians participating in a MIPS APM. For this option, you report a predetermined set of Quality measures as well as the complete Promoting Interoperability measure set. Participants currently receive full credit in the Improvement Activities performance category, although this is reevaluated annually; Cost is not evaluated.
Practice Fusion’s Electronic Clinical Quality Measures (eCQMs) Dashboard
Practice Fusion’s eCQM Dashboard is an intuitive hub for Quality measure tracking that allows you to monitor progress in multiple quality programs, including MIPS. eCQMs use data extracted electronically from your Practice Fusion electronic health record (EHR) to measure the quality of health care provided to your patients. The specific number of Quality measures you’re required to report depends on your selected MIPS reporting
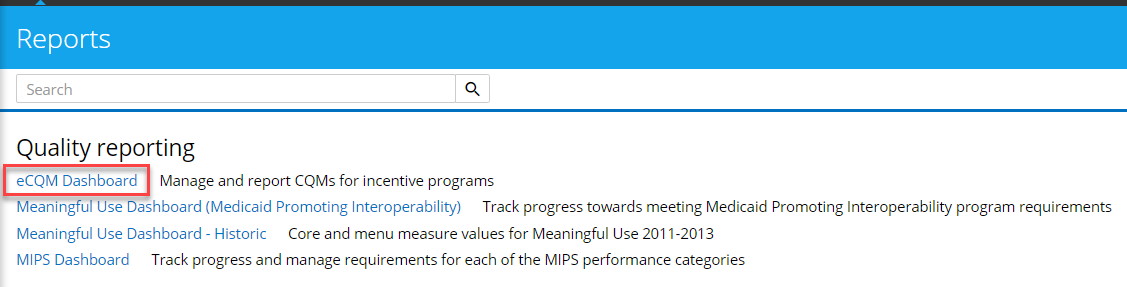
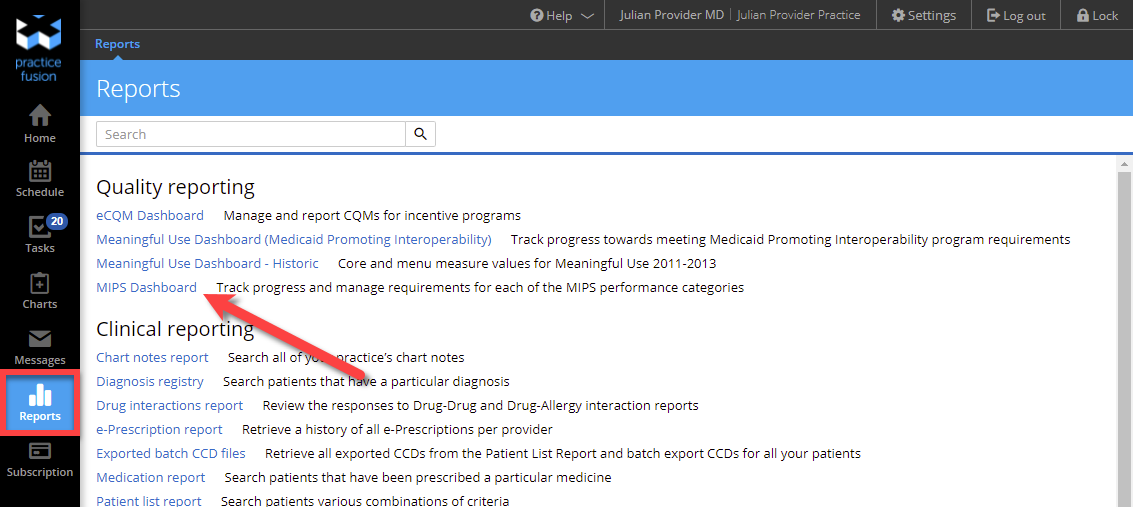
To access the eCQM Dashboard, click the eCQM Dashboard link, which can be found under the Quality reporting header on the Reports page.
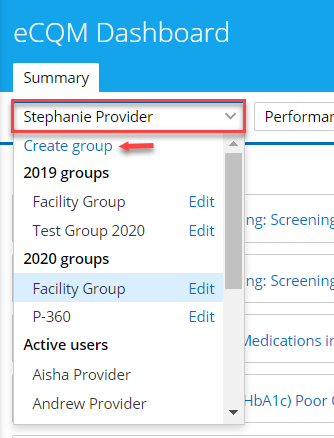
Select the name of an eligible clinician from the left drop-down menu. Or, if you plan to report as part of a group, select Create Group.
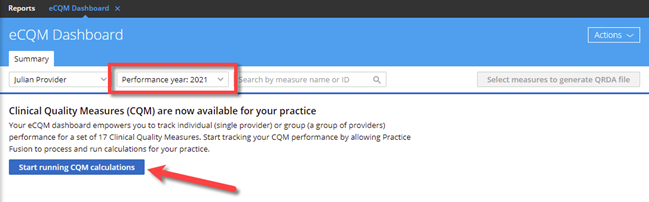
Select the performance year from the right drop-down menu. Note: If you have not yet opted to run performance calculations for this performance year, you need to click Start running CQM calculations; it may take up to 48 hours to generate up-to-date scores.
To ensure that Practice Fusion supports your selected Quality measures, review a complete list of eCQMs Practice Fusion supports for 2024 and the suggested Practice Fusion workflow for each measure.
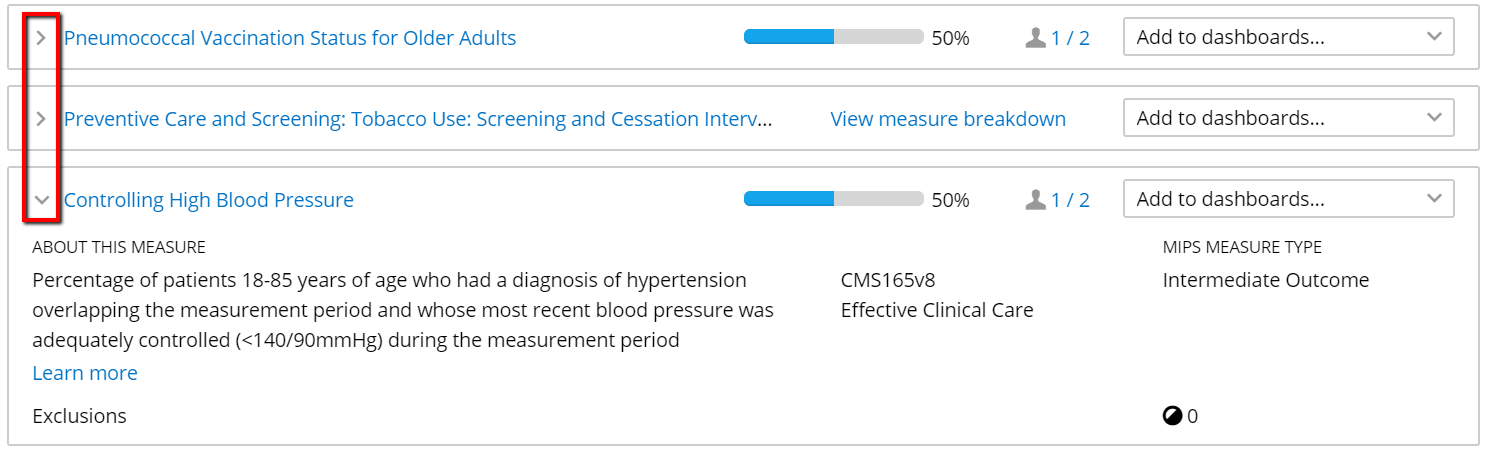
To review specific Quality measures, you can scroll through the eCQM list or search by measure name or CMS ID number. To learn more about a particular measure, click the drop-down arrow at the measure’s left to view more detailed information; alternatively, click Expand all measures at the top right to view more detail for all listed measures.
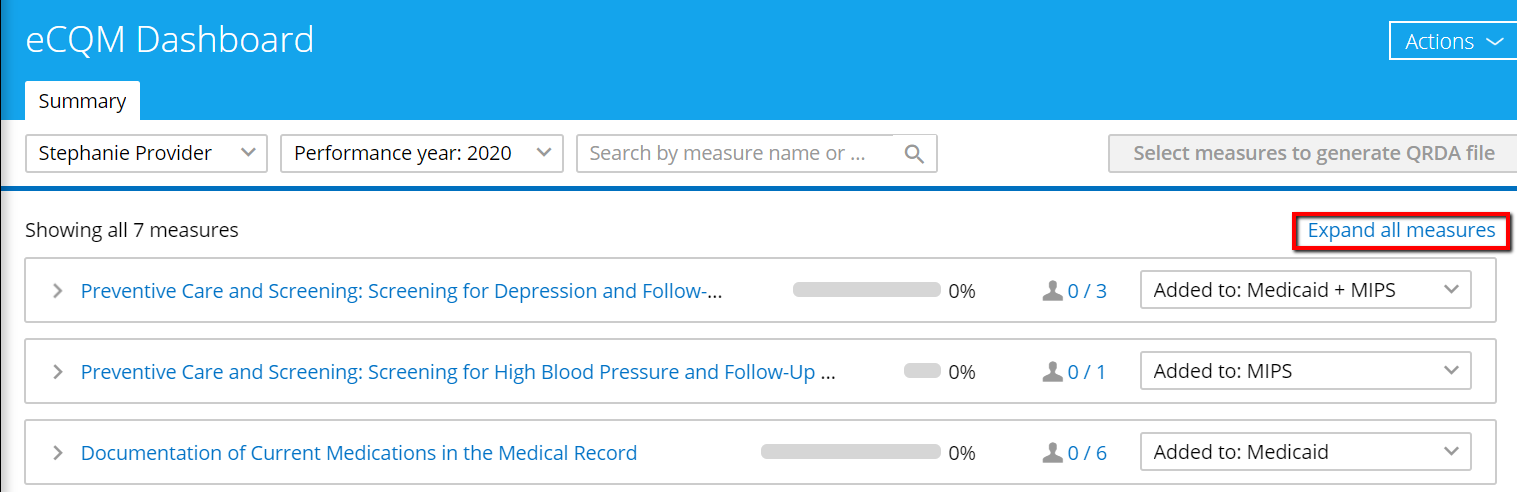
Each measure will display a progress bar beside the measure name, showing the calculated percentage based on Numerator/Denominator values for that measure. These bars update every 48 hours.
Check current MIPS settings
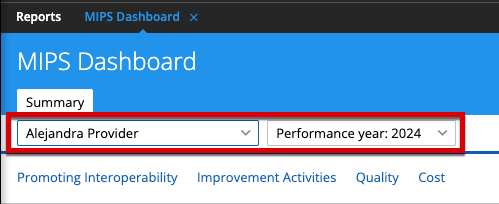
In preparation for MIPS reporting, ensuring that your system is correctly set up for the 2024 MIPS performance year is essential. You can check your current MIPS settings using the Practice Fusion MIPS Dashboard, an easy-to-manage tool that enables you to track progress in 3 of the MIPS performance categories. You can access the MIPS Dashboard from the Reports section: Click MIPS Dashboard under the Quality reporting heading.
To check your current MIPS settings, select your name and current performance year at the top of the screen, then click the MIPS settings link at the top right:
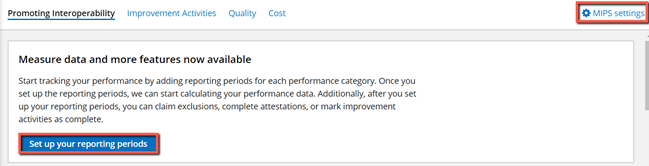
Here, you can confirm that the reporting period date ranges have been set up correctly for each MIPS category:
- Promoting Interoperability reporting period: Full year or custom option (180 days)
- Improvement Activities reporting period: Full year or custom (90 days)
- Quality reporting period: Full year is the only option
Check the details
Quality
Certain details must be addressed and tasks completed before the Dashboards can correctly track your MIPS performance. For instance, you must remember to sign off on your patient encounter notes. Only signed chart notes will be included in calculations for your chosen Quality measures.
In addition, patients will receive access to their electronic healthcare information via the Patient Portal only after you’ve signed their chart notes—an essential element of the Promoting Interoperability measures. As a result, failure to sign chart notes can also negatively impact the Promoting Interoperability performance category.
Promoting Interoperability
Another essential detail to check during your MIPS end-of-year check-in: Have you completed the Security Risk Analysis? This assessment must be completed once a year, before the end of the MIPS reporting period.
The Office of the National Coordinator for Health IT (ONC) provides a Security Risk Analysis tool to help practices perform and document a comprehensive risk assessment within their organizations. Click here to download the ONC Security Risk Analysis tool.
Check your patient population
It’s also important to check which patients were included in the patient population (the Denominator used for Quality measure calculations) and whether those patients were also included in the Numerator. For patients not included in the Numerator, check their encounters that fall in the current measurement period to verify that the suggested workflow was followed, which will ensure it will be included. (Suggested workflows can be found in the Knowledge Base articles for each Quality measure.)
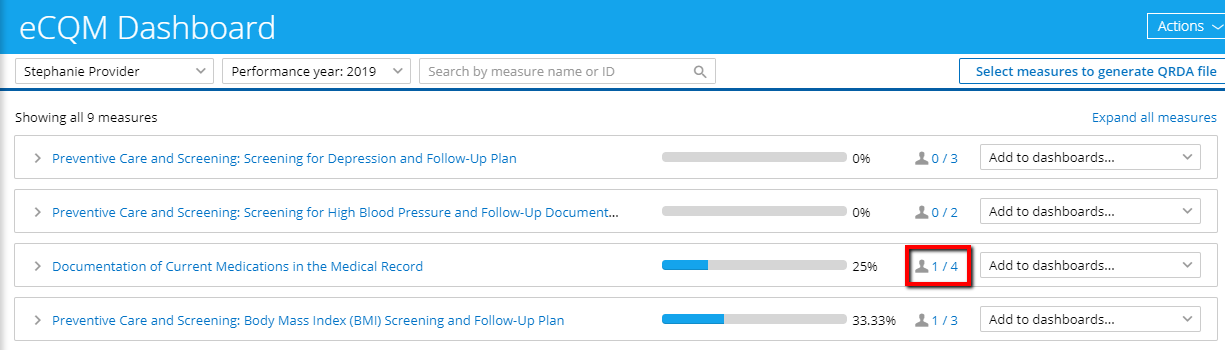
Patient population information can be checked using the Patient Report link on the eCQM Dashboard. When viewing measure information, click the blue patient numbers to the right of the desired measure to see the Patient Report for that specific Quality measure.
The Patient Report lists individual patients included in the patient population for that measure and patient contact information to streamline any downstream communications that might be needed to fulfill measure requirements. The Patient Report also includes the initial patient population for each measure, patients included in the Numerator and Denominator, and any applicable exclusions or exceptions.
Check-in for MIPS success
To get the most from your MIPS participation, it’s critical to ensure your EHR and MIPS reporting system contain all required information and is correct and up-to-date. Reviewing the key points covered in this article will help you ensure you submit accurate and complete data to support your final MIPS score.
If you don’t have Practice Fusion and you are interested in learning more about how we can help you make the most of your MIPS requirements, contact us today!
