How to connect Health Information Exchange (HIE) with Electronic Medical Records
Health information technology (health IT) is seen as central to improving healthcare delivery, and is the focus of the HITECH section of the American Recovery and Reinvestment Act (ARRA) of 2009 (which sets up and funds bonuses for Meaningful Use of Certified EHR technology). A key element in order for this to work well is the safe, secure interchange of patient-centric health data between different settings of care.
Given that traditional Electronic Medical Records (EMR) systems have been built for local installation in a doctor’s office, clinic, medical group or hospital, patient information does not natively flow between these settings. The traditional view of EHRs is that they are supposed to be all-inclusive enterprise solutions that function within the closed walls of a secure network. As such, the organization of health information across the landscape is not much different than it was when paper was used as the method to store information – each setting of healthcare kept its own medical records system. Given that patients see, on average, 18.7 different doctors (not counting hospitals, labs, x-ray departments, etc), fragmentation of health information is inevitable.
So, how will patient-centric information flow between these different setting, given that each setting may use completely different EHR systems that internally manage health information completely differently? The main approach to date has been to package standardized files (Continuity of Care Documents, or CCDs; or Continuity of Care Records, or CCRs) and send them back and forth across secure connections. In fact, the ability to do this is a Certification requirement for products that can be used for Meaningful Use.
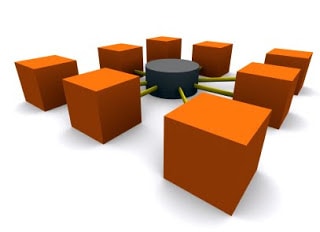
Connecting every doctor’s office with every other health setting (like local hospitals, other doctor’s offices, labs, and so forth) with a myriad of one-to-one connections is overwhelmingly complex, and perhaps impossible to do on a scale as envisioned by HITECH. To simplify this connectivity, then, regional Health Information Exchanges (HIEs) have emerged, to act as hubs – a doctor only needs to connect the in-house EHR to a single hub, and through that center connectivity with all other subscribers to that hub can be obtained.
 HIEs, therefore, act much like a clearinghouse for clinical information. Clearinghouses have been around for quite some time, mainly in the realm of submitting billing information to insurance companies. Medical billing clearinghouses act as hubs that receive electronic bills from the Practice Management systems used by doctors’ offices (or their billers), scrub them for data accuracy (make sure there are valid dates in required fields, valid codes where they belong, etc.), and then pass them along to the insurance payors. Billing software needs to subscribe to a medical billing clearinghouse (there are many), which means going through a testing procedure to make sure it all works. Often physicians are not aware of all this back-end connectivity, but billers certainly are.
HIEs, therefore, act much like a clearinghouse for clinical information. Clearinghouses have been around for quite some time, mainly in the realm of submitting billing information to insurance companies. Medical billing clearinghouses act as hubs that receive electronic bills from the Practice Management systems used by doctors’ offices (or their billers), scrub them for data accuracy (make sure there are valid dates in required fields, valid codes where they belong, etc.), and then pass them along to the insurance payors. Billing software needs to subscribe to a medical billing clearinghouse (there are many), which means going through a testing procedure to make sure it all works. Often physicians are not aware of all this back-end connectivity, but billers certainly are.
Another example of a clearinghouse is Surescripts – this is the main hub through which electronic prescriptions are channeled. EHR systems (or stand-alone eRx systems) send prescriptions to Surescripts, which then forwards it to local pharmacies. Physicians don’t have to worry about establishing connections with each and every local pharmacy – so long as the EHR can connect to Surescripts, then connectivity with all participating pharmacies takes place. The enrollment process with Surescripts is also a process which an EHR vendor must go through.
HIEs, therefore, are basically clearinghouses for exchange of clinical data. Apart from the technical issues of assuring that everyone using the HIE submits data in a standardized format, and uses standardized vocabulary (this is actually a herculean task, and is far from universal, currently), there is the question of how an HIE will support itself as a business.
Medical billing clearinghouses charge for their services – either an annual fee, or a per-transaction charge. These charges pass back to the physician practice (or the biller’s cost), either as direct cost or as an item rolled into a software vendor ongoing support fee. Surescripts is funded by participating retail pharmacies and Pharmacy Benefits Managers (PBMs), given that is lowers their overhead to have prescriptions come in electronically directly into their systems.
So how will HIEs support themselves? Under HITECH, a total of $547 million has been allocated by the Office of the National Coordinator (ONC) to 56 different HIEs to help their efforts to rapidly build capacity, and help evolve the necessary governance and policy issues around exchange of protected health information in a safe and private way. This is development seed money, not ongoing production money.
A number of questions remain uncertain when it comes to HIEs as viable future going-concerns. Will they charge users for access, much like how medical billing clearinghouses do? If there are charges for use of an HIE, will these be passed on to an EHR vendor, who rolls these charges into ongoing service and support fees to physician end-users (much like how medical billing clearinghouses do)?
A web-based EHR basically has a built-in free HIE for users within its system, regardless of location. Connectivity with these ONC-funded regional HIEs will be needed for connectivity to legacy systems (plus, it is a Certification requirement), but exactly how the business relationships should be remains an unanswered question.
For the time-being, HIEs, subsidized by public money for proof-of-concept development, will offer connectivity in an open way. However, how these entities will function down the road remains to be seen.
Robert Rowley, MD
Chief Medical Officer
Practice Fusion EMR



